Guest Blogger: How SARS-CoV-2 Impacts the Body by Dr. Stephanie Langel
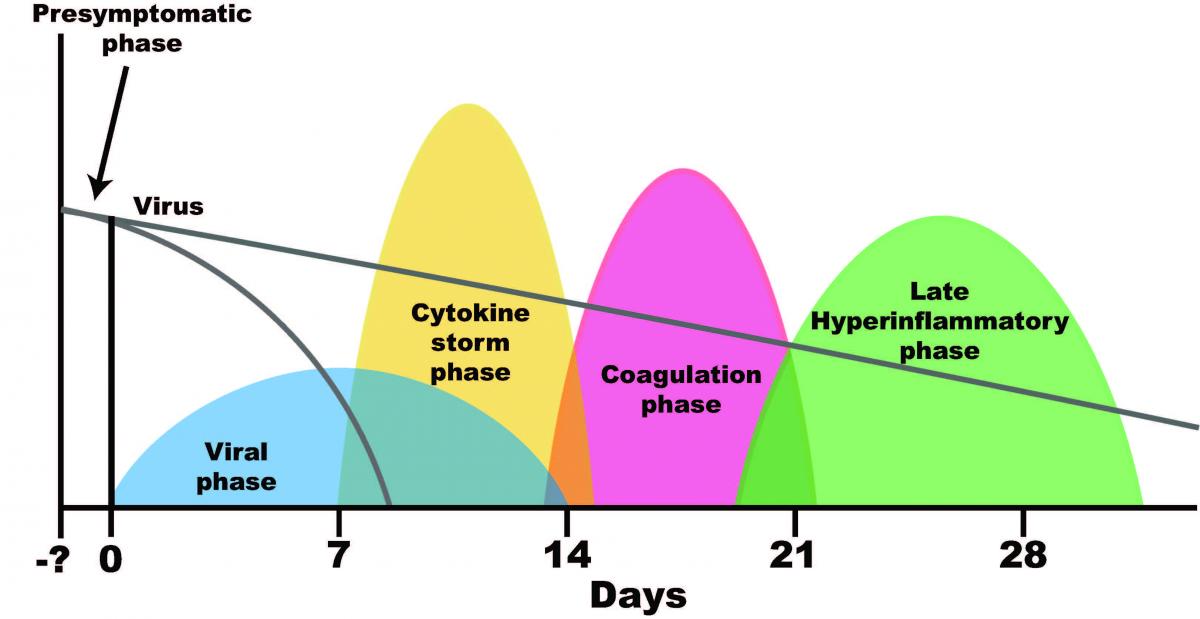
I want to explain about the phases of the disease that medical doctors are seeing in symptomatic COVID-19 patients. I also want to address how someone can die of COVID-19 (the disease) even after they have cleared SARS-CoV-2 (the virus) from their body.
Let’s start from the beginning. SARS-CoV-2 is spread from respiratory droplets during exhalation (breathing, speaking, singing, coughing, sneezing). After the virus gets into your mouth, nose and maybe even the eyes, it is looking to bind to something called a receptor sitting on the surface of your cells. Think of it as a key looking for its keyhole. Once the virus (the key) binds to its receptor (the keyhole) it can enter your cells (your house) and start replicating (aka making copies of itself). This brings us to the first phase of the disease; the viral phase.
During the viral phase, SARS-CoV-2 is making more and more copies of itself until it peaks somewhere within the first week after initial infection. While this is happening, your body’s cells (including immune cells) immediately recognize something is wrong and start producing small communication molecules called cytokines. Cytokines are one of many proteins that your body produces to send out an “SOS” signal to your immune cells. Your immune cells receive the message and kick into high gear. They migrate to the site of infection to start killing virus infected cells. This process is ‘proinflammatory’ and ultimately leads to inflammation.
Inflammation is mostly thought of in a negative way. However, proinflammatory responses at the beginning of an infection are absolutely necessary to keep us alive. Rising body temps (aka fever), aches, chills, fatigue are a result of proinflammatory cytokines. In a normal immune response, your body would respond to these “SOS" signals, recruit immune cells to the site of infection (in this case, the lung), kill virus infected cells and then the healing process begins. To heal, your body must transition from a proinflammatory phase and into a regulatory phase; the regulatory yin to the proinflammatory yang. If you can’t get out of the proinflammatory phase, you’re going to have issues. This leads us to the second phase on the graph; the cytokine storm phase.
A cytokine storm is when your body is reacting so strongly that the cytokine production at the site of infection ramps up and spills into your blood. This is a problem. High levels of cytokines in your blood can cause high fever, swelling and redness, extreme fatigue and nausea. In some individuals (and more likely in those with preexisting health conditions) this cytokine storm causes more severe symptoms including blood vessel leakage, a drop in blood pressure, clot formation and organ failure. As you can notice from the graph, by the time there is an increase in cytokines in blood, the levels of virus in your body may have gone down and may even be undetectable. The problem is that even though the virus is on its way out, your body isn’t done responding to it. It hasn’t found the off switch yet. This is why an infected individual can no longer have detectable virus but still have complications and even die several weeks later.
Remember, cytokines are signals to your body to react quickly. One of the signals that cytokines communicate is to tell your blood vessels to dilate. This helps immune cells migrate from your blood to your tissues where the infection is happening. However too many cytokines mean too much blood vessel leakage. Your body has a solution to every problem and in this case, the solution is to clot. This brings us to the third phase: coagulation.
The clotting cascade in your body senses the increase in vascular leakage, freaks out and starts working overtime to clot all of the leaky spot in your blood vessel walls. You can imagine how big of a problem it can be for people with clotting issues. Many people are dying of COVID-19-related clotting issues including stroke, congestive heart failure and kidney failure. You can see from the graph that coagulation issues are happening weeks after the onset of symptoms and possibly even after the body has cleared the virus. The virus has done its job and has moved on to infect the next person, but the patient is still dealing with the consequences of having developed a response to the virus that was too strong.
I was having a conversation with someone whose family friend had died of congestive heart failure. This man went to the hospital weeks earlier because he was experiencing COVID-19 symptoms (fever/chills, coughing, shortness of breath, fatigue) and upon arrival, tested positive for SARS-CoV-2. Approximately three weeks after he was admitted, he developed congestive heart failure and died. At this time he was negative for SARS-CoV-2. The person I was speaking with assumed this meant his friend did not die of COVID-19. Once I showed him this graph, I was able to convince him that viral infections can cause hyperinflammation leading to long term sequela (aka long-term effects) and possibly death including congestive heart failure...even after testing negative for SARS-CoV-2.
This leads us to phase IV or the ‘late hyper inflammatory phase’. This is probably the least understood phase of COVID-19 and in some patients, and it lasts much longer than one month post symptom onset. People who are experiencing the long-term negative effects of a COVID-19 infection have named themselves ‘COVID long-haulers’ and have formed support groups on reddit, twitter, Facebook and other social media channels to try to understand why they feel crappy and are having difficulties doing basic tasks. The experience of COVID-19 long haulers mirror what people with chronic illnesses deal with day-in and day-out. I have talked to a couple ‘long-haulers’ who have become much more sympathetic to people with chronic illness because it’s a constant uphill battle to get your family, friends and even doctors to believe that something is wrong with you and you are not just “being lazy”. Many COVID-19 long-haulers are young and had no previous health conditions prior to getting the disease.
I hope by writing this people will get an idea of what medical doctors are seeing in the hospital. Also, I hope you will have better understanding of the immune response to a viral infection and of how an unbalanced (too strong) immune response to SARS CoV-2 can lead to complications and even death in some COVID-19 patients after the virus is gone.
I often feel like I’m living in two worlds, one world where I wear a mask and social distance and I am on conference call after conference call listening to doctors and scientists talk about the negative impacts of the disease. This is a stark contrast to when I hear people say that we should let “the virus spread unmitigated” to “build herd immunity”. Unfortunately, with a coronavirus (or any virus for that matter), “herd immunity” is not something we can accomplish without a vaccine. Those who suggest this as a strategy don't understand coronavirus pathogenesis or the development of adaptive immunity through memory B and T cell generation. Letting the virus spread through the population unchecked will lead to many more thousands of otherwise preventable deaths.
So, to protect our most vulnerable while making sure people can work and kids can go to school, we must work together. To prevent community transmission of this virus it is important to wear face masks and practice social distancing. Winter is coming and that means being indoors more, less ventilation, closer contact - perfect conditions for spread of respiratory viruses. As you make your holiday plans, my hope is that you remember this graph and make choices that decrease the potential for virus spread. It is possible to keep our communities safe if we work together to protect ourselves and those around us.
Graph: The graph was created by Dr. Daniel Griffin, MD, PhD and I was given permission to share it on social media. Daniel Griffin,MD, PhD is a member of the Division of Infectious Diseases and an Associate Research Scientist in the Department of Biochemistry and Molecular Biophysics at Columbia University. Dr. Griffin has treated hundreds of COVID-19 patients as a physician in New York City and gives weekly updates regarding the clinical aspects of COVID-19 on a podcast called 'This Week in Virology' (www.microbe.tv/twiv).
Stephanie Langel, PhD is a postdoctoral fellow in the lab of Dr. Sallie Permar studying maternal and neonatal immunity and mucosal vaccination strategies for prevention of enteric and respiratory diseases. She also contributes to a monthly podcast ‘Immune’ about the body’s immune system (www.microbe.tv/immune)